Late in 2022, beloved actress Christina Applegate opened up about her battle with Multiple Sclerosis (MS) and how it has turned her life upside-down. Her courage to share her difficult journey has brought renewed attention to this devastating and complex disease.
MS is a ruinous disease that affects the central nervous system, which includes both the brain and the spine, but not the peripheral nervous system.
Blog Contents
- Why does Multiple Sclerosis happen?
- How common is Multiple Sclerosis?
- Which risk factors can cause Multiple Sclerosis?
- What are the symptoms of Multiple Sclerosis?
- How is Multiple Sclerosis diagnosed?
- How is Multiple Sclerosis treated?
- Can lifestyle changes reduce Multiple Sclerosis complications?
- What is the future of Multiple Sclerosis treatment?
Why does Multiple Sclerosis happen?
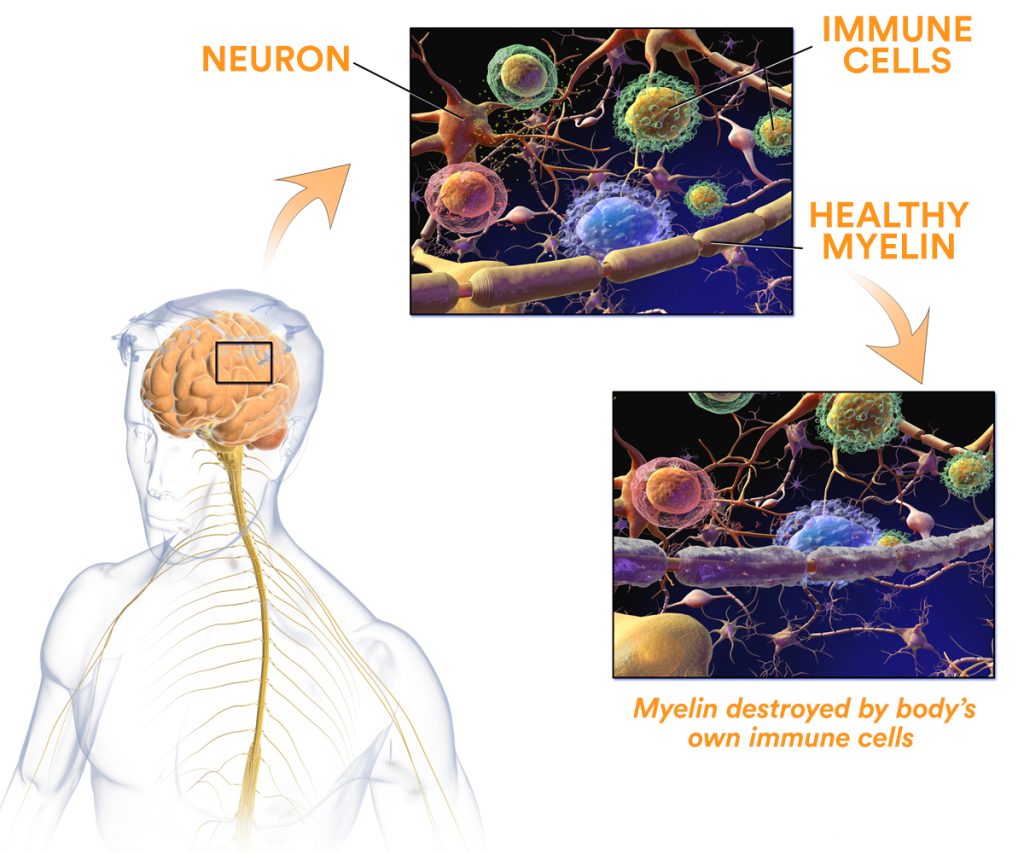
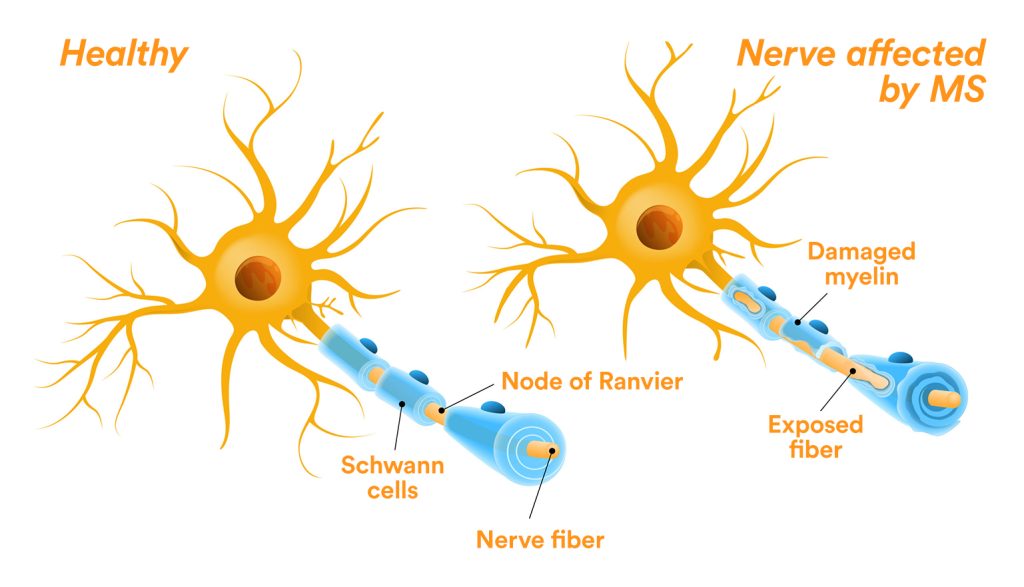
Multiple Sclerosis is caused by the immune system attacking the sheath covering the connections between neurons — these are called axons — and the insulation around them, known as the myelin sheath.
The result is serious communication problems between different neurons and entire sections and systems in the brain.
Originally described by Charcot, the pathology associated with ‘sclerose en plaques’ has been shown to affect the periventricular area, brain stem, and spinal cord.
The inflammatory infiltrating substances contain particular immune cells called T-lymphocytes (CD8), with further damage taking place as a result of secondary inflammation. Early on, the axons are preserved, but as the disease progresses, they also become irreversibly damaged.
How common is Multiple Sclerosis?
In the United States, MS is the most common disabling neurological disorder among young adults.
It affects more than 2.3-million people worldwide, making it the most frequently-seen demyelinating disease.
Its prevalence varies considerably, with high levels in North America and Europe (about 300/100,000 people) and low rates in Eastern Asia and sub-Saharan Africa (2/100,000 people).
Which risk factors can cause Multiple Sclerosis?
Age
The highest risk is among people aged 15-29, with the greatest increase occurring between the ages of 15 and 19.
Race and Gender
Women have a higher risk than men, and Caucasians of Northern European descent have a higher risk than other racial/ethnic groups.
Location and Migration
Studies have shown that the risk of developing MS increases with age and latitude (above 35°N).
Interestingly, if someone moves from a higher latitude to a lower one before the age of 15, their risk of developing MS decreases.
However, if they move after the age of 15, their risk does not decrease significantly.
Environmental Factors vs. Genetics
Migration studies consistently support MS being secondary to an environmental exposure. Adult migrants from low-risk countries (such as the West Indies) to Europe are at low risk of developing MS. However, children born to migrants in Europe are at high risk.
This indicates that environmental factors may trump genetics and argues strongly for prevention studies targeting known environmental risk factors.
To date, several factors have been associated with an increased risk of developing MS. Epstein-Barr virus (EBV) and Herpesvirus 6 infection, especially if they occur after childhood and are symptomatic, have been shown to increase the risk.
Smoking is another environmental factor that increases the risk of developing MS.
Genetic factors also play a role in MS susceptibility, with about one in eight MS patients having a family history of the disease. However, vaccines, stress, traumatic events, and allergies have not been identified as risk factors.
Nutrition
Recent studies have found evidence for a role of vitamin D and obesity as independent risk factors causing MS.
MS risk modification occurs throughout life, starting in utero. The month of birth is correlated with an increased concordance, and hormonal abnormalities, such as estrogen and testosterone levels, have been linked to MS.
Women with higher levels of estrogen may be at an increased risk of developing the condition.
Nutritional deficiencies, such as vitamin D and omega-3 fatty acid levels, may also contribute to the development of MS.
Epidemiologic data has revealed that MS may slightly shorten life expectancy by six years. Preventative approaches might be derived from knowledge of the risk factors and natural history of the disease (smoking, vitamin D).
What are the symptoms of Multiple Sclerosis?
Multiple Sclerosis (MS) is a complex disease with various classifications. These include Clinically Isolated Syndrome (CIS), Relapsing-Remitting, and Secondary Progressive MS.
CIS refers to the first episode of neurological symptoms caused by inflammation and demyelination in the central nervous system.
Its duration should be at least 24 hours, and symptoms vary but commonly include optic neuritis, vertigo, loss of sensation in the face, weakness in the arms and legs, ataxia, and bladder problems.
The most common disease course is Relapsing-Remitting MS (RRMS), accounting for around 85% of people with MS.
This course is characterized by new or increasing neurological symptoms followed by periods of recovery or remission.
When the disease course does not have a recovery period and continually progresses, it is considered to be Secondary Progressive, in which disability accumulates over time.
There are also variants of MS, including Devic’s disease, Balo’s concentric sclerosis, Schilder’s syndrome, and Marburg MS, each with unique symptoms and disease progression.
How is Multiple Sclerosis diagnosed?
Diagnosis of MS is based on a combination of clinical findings, imaging, and laboratory data using the current diagnostic criteria known as the Revised McDonald Criteria.
MRIs play a crucial role in providing information about the disease’s state and progression.
Another essential tool is Lumbar puncture and detection of specific immunoglobulin proteins (oligoclonal bands).
How is Multiple Sclerosis treated?
While there has been tremendous progress in treating MS, currently, there is no cure.
However, there are many disease-modifying drugs that can reduce the frequency and intensity of the disease and the relapses.
These drugs can be divided into two categories: disease-modifying therapies (DMTs) and symptomatic therapies.
DMTs are MS-specific and reduce the frequency of relapses and short-term disability. Injectable medications such as interferons and glatiramer acetate reduce the relapse rate by 29% to 34% compared with placebo.
Oral medications such as S1P modulators, fumarates, and teriflunomide vary in their effects on relapse reduction, ranging from 36% to 58% over 2 years.
Most of the DMTs have been approved for use only in relapsing forms of MS and some for secondary progressive disease.
The DMTs currently approved by the US Food and Drug Administration (FDA) include interferons, S1P receptor modulators, monoclonal antibodies, and miscellaneous immunomodulators.
However, adverse side effects of these drugs can include infections, bradycardia (slow heart rate), other heart conditions, macular edema, and autoimmune reactions.
It is important for patients to discuss the risks and benefits of these medications with their healthcare provider.
Can lifestyle changes reduce Multiple Sclerosis complications?
There is some evidence of lifestyle interventions such as exercise and nutrition being helpful in reducing relapses.
Higher Mediterranean diet alignment has been shown to predict lower objective and patient-reported disability.
The WHO recommends no more than 5% of dietary calories should be consumed as sugar.
In general, a varied diet rich in unprocessed foods is recommended, but there is need for much more robust studies looking at the long-term benefits of lifestyle on disease course.
Concurrently, claims of efficacy for herbal remedies, bee venom, or certain vitamins have never been demonstrated.

What is the future of Multiple Sclerosis treatment?
The future of MS treatment is on an exciting path of discovery, with two different approaches leading the way.
One direction is the preventive path, which focuses on risk factors such as the environment and lifestyle.
Researchers are learning more and more about the different components, such as the role of genetic risk, infectious agents, and lifestyle choices and their contribution to MS.
The second approach is focused on treating MS at the point of diagnosis. This approach involves adjusting the immune system to prevent it from attacking the myelin sheath and reducing secondary inflammation.
This cutting-edge technique is proving to be very promising in the fight against MS. With two different approaches to the treatment of MS, the future looks bright.
Researchers and medical professionals are committed to finding a cure and improving the lives of those affected by this debilitating disease.
This disease needs the voice of brave advocates like Christina Applegate who can speak about their journey with the disease and in doing so help raise awareness and marshall resources for the fight.



