Parkinson’s is a devastating progressive neurological disorder that affects the central nervous system. It is a debilitating condition that can cause a person to experience a variety of physical, cognitive, and emotional symptoms.
While the cause of Parkinson’s is still unknown, numerous treatments and lifestyle interventions are available to help manage the symptoms and improve the quality of life for those affected.
In this article, we will discuss the definition and epidemiology of Parkinson’s disease, the proposed scientific causes, treatments, lifestyle interventions for prevention and treatment, current innovative science, and the future of Parkinson’s treatment.

What is Parkinson’s disease?
Parkinson’s is caused by the gradual loss of neurons in the brain that produce the neurotransmitter dopamine.
Dopamine helps to regulate movement, coordination, and motivation, so when it is depleted, the person experiences a variety of physical, cognitive, and emotional symptoms.
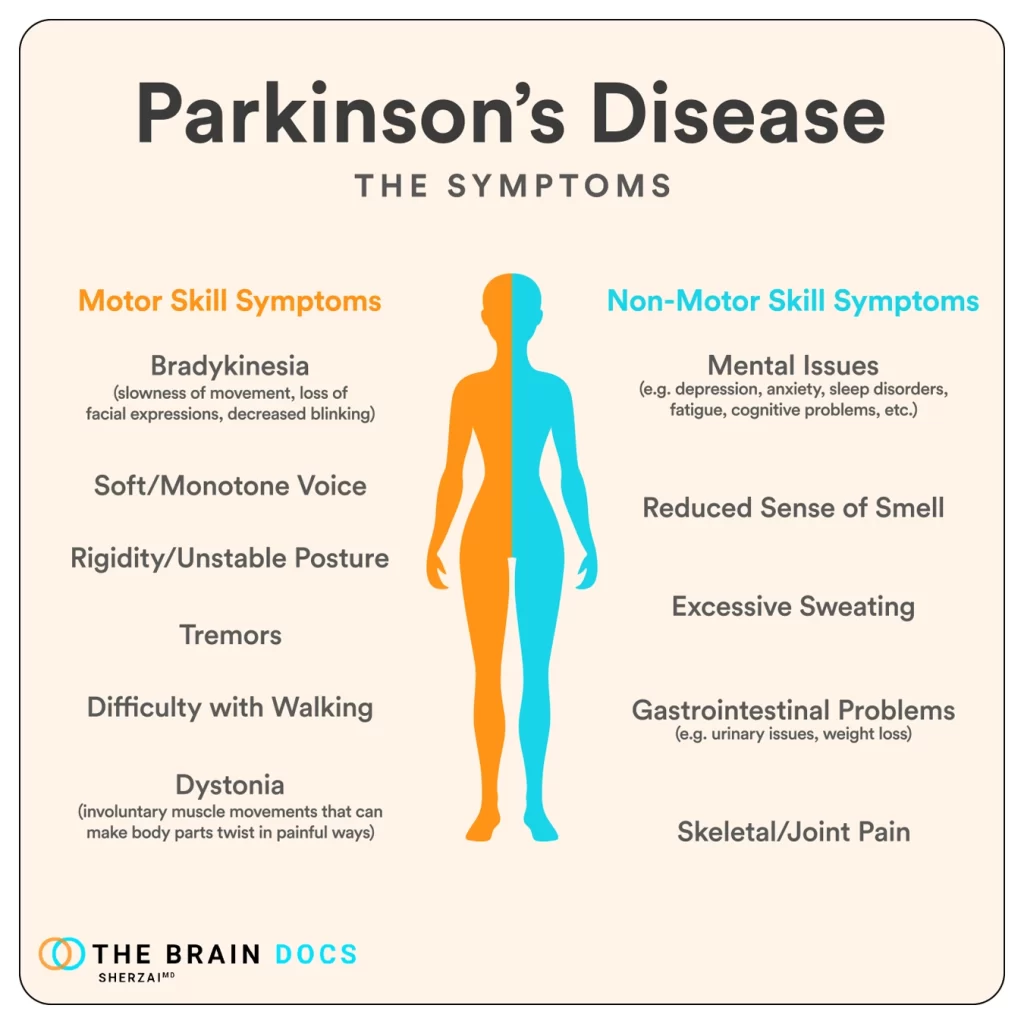
These can include tremors, rigidity, slowed movement, impaired balance, difficulty with speech, thinking, motivation, swallowing, and mood changes.
How common is Parkinson’s?
Parkinson’s disease is the second-most-common neurodegenerative disease after Alzheimer’s disease. It affects approximately 1-million people in the United States, and an estimated 60,000 new cases are diagnosed each year. Worldwide, more than 10-million people suffer from Parkinson’s disease.
It impacts approximately 1% of the population over the age of 60, although there are younger cases like Michael J. Fox, who developed the disease at age 29.
Men are more likely to be affected than women. Most studies report the highest prevalence of PD in white populations (1,671.63/100,000, compared with 1,036.41/100,000 in Black populations, and 1,138.56/100,000 in Asian populations).
Janet’s Story
Janet had been feeling off for months. She was having difficulty sleeping, her hands were shaking, and she was having trouble focusing. She went to her doctor and they ran some tests, but they couldn’t find anything wrong.
They told her it was probably just stress and that she should take some time off work to relax. However, the symptoms didn’t go away, and Janet was getting increasingly worried.
She went to a specialist to run more tests, but they still couldn’t find anything wrong. Finally, after months of doctor visits, Janet was diagnosed with Parkinson’s Disease.
The diagnosis was devastating. She was scared and confused, and she had no idea what to do next. She started researching the disease and trying to find the best treatments available, but the treatments were expensive and she had no idea how she was going to afford them.
Janet had to make some tough decisions. She had to quit her job and start relying on her family for help. She was embarrassed and ashamed, but she had no other choice.
The treatments were difficult and exhausting. She had to take a variety of medications and go to regular therapy sessions. She also had to make lifestyle changes, like eating a healthier diet and exercising regularly.
It was an incredibly long and difficult journey, but Janet was determined to fight the disease. She kept going and eventually she started to see improvements. She was able to manage her symptoms and live a relatively normal life.
But the disease was always there, lurking in the background. It was a constant reminder of the difficulties she had faced and the struggles she had gone through.
She was determined to keep fighting, but it was never easy. Janet’s story is one of strength and resilience. Despite the difficulties she faced, she was able to find the courage and determination to keep going.
Eventually, she was able to find the right treatments and manage her symptoms, and she was able to live a full and meaningful life.
What causes Parkinson’s disease?
The exact cause of Parkinson’s disease is still unknown, but there are several proposed scientific causes, such as genetic risk, toxins, environmental factors, oxidative stress, traumatic brain injury, vascular, pharmaceutical, or a combination thereof.
But recent research has shown that genetics plays a significant role in the development of Parkinson’s disease. The Parkinson’s Foundation reports that about 15% of people with Parkinson’s disease have a family history of the disease.
In addition, recent studies have identified several genetic mutations that increase the risk of developing Parkinson’s disease. For example, a study published in the journal Nature Genetics in 2020 identified a new genetic variant associated with an increased risk of Parkinson’s disease.
Environmental factors are also thought to play a role in the development of Parkinson’s disease. Exposure to certain chemicals, such as pesticides and herbicides, have been linked to an increased risk of developing the disease.
A study published in the journal Movement Disorders in 2020 found that exposure to pesticides was associated with a higher risk of developing Parkinson’s disease.
How is Parkinson’s treated?
There is no cure for Parkinson’s disease, but there are several treatments available to help manage the symptoms. These include medications, physical therapy, and surgery.
Medications can help to reduce the symptoms of Parkinson’s by increasing release of dopamine, or breakdown of dopamine or effect on other neurotransmitters that will directly or indirectly influence movement, while physical therapy can help to improve mobility and balance.
Surgery — specifically implantation of wires in the thalamus or basal ganglia — can drastically (at least temporarily) improve movement and rigidity, and can help with other symptoms.
This is a remarkable procedure to see, as during the process, one actually raises the electricity level in a particular location and in front of your eyes you see a person’s tremor go away.
This procedure has been life-altering and has given people with Parkinson’s years of better quality life, but it does nothing in slowing the natural cause and ultimate outcome of the disease.

Can Parkinson’s be prevented?
At this time, we have symptomatic treatments such as medication, surgical interventions, physical therapy, occupational therapy, and speech therapy — but there has been very little focus on prevention.
One especially helpful tool has been ‘BIG therapy’, which works on the patient by greatly exaggerating their movements, writing, and speaking. In doing so, they are able to actually come close to accomplishing activities as they might have before the onset of Parkinson’s.
In addition to medications and physical therapy, there are several lifestyle interventions that can help to improve the symptoms of Parkinson’s disease.
Research has shown that various factors, including nutrition, lifestyle, and and other epi-genetic factors play a role in the development and prevention of Parkinson’s disease.
A healthy diet rich in vitamins and minerals (such as vitamin E and vitamin D) and folic acid, alongside regular physical activity and moderate caffeine consumption, may help reduce the risk of developing Parkinson’s.
Additionally, reducing exposure to environmental toxins and pesticides could lower the risk of Parkinson’s. However, the complex interplay between these factors and genetic susceptibility remains unclear, necessitating further research to develop personalized prevention strategies based on individuals’ genetic risks.
Other factors such as regular exercise, eating a healthy diet, getting enough sleep, and avoiding alcohol and smoking may also reduce the risk for developing Parkinson’s. But much more research is needed to clearly delineate these relationships.
Innovation in Parkinson’s research
There is a great deal of research being done on Parkinson’s disease, and there are several innovative treatments being developed.
One such treatment involves a new approach to stem cell therapy that replaces the dopamine-producing cells that are lost in the disease.
Another promising treatment is gene therapy, which involves using viruses to deliver therapeutic genes to the brain, as well as much more novel electronic approaches to the disease.
There is also a growing focus on personalized medicine, which involves tailoring treatment to the individual patient based on their unique genetic and environmental factors.
These treatments are still in the early stages of development, but they hold promise for improving the quality of life for those affected by Parkinson’s.
The future of Parkinson’s treatment
The future of Parkinson’s treatment is very promising.
With continued research and the development of innovative treatments, it is likely that more effective treatments will become available in the future.
Additionally, lifestyle interventions will continue to play an important role in managing the symptoms of Parkinson’s disease.
To summarize, Parkinson’s disease is a progressive neurological disorder caused by the loss of dopamine-producing neurons in the brain.
It affects approximately 1-million people in the United States and more than 10 million people worldwide.
The exact cause is still unknown, but genetics, environmental factors, and oxidative stress are thought to play a role.
There is no cure for Parkinson’s disease, but there are several treatments available to manage symptoms, including medications, physical therapy, and surgery.
Lifestyle interventions such as exercise, healthy eating, sleep, social activity, and stress management can also help manage symptoms.
There are several innovative treatments being developed, including stem cell therapy, gene therapy, and personalized medicine, that hold promise for improving the quality of life for those affected by Parkinson’s disease.
So, for people all over the world like Jane living with Parkinson’s disease and their loved ones, know that you are not alone.
There are millions of others who are fighting this battle alongside you, and together, we can continue to raise awareness, support research, and ultimately, find a cure.
Sources
Gao, X., Cassidy, A., Schwarzschild, M. A., Rimm, E. B., & Ascherio, A. (2020). Habitual intake of dietary flavonoids and risk of Parkinson disease. Neurology, 94(16), e1646-e1654.
Maraki, M. I., Yannakoulia, M., Stamelou, M., Stefanis, L., Xiromerisiou, G., Kosmidis, M. H., … & Scarmeas, G. P. (2019). Mediterranean diet adherence is related to reduced probability of prodromal Parkinson’s disease. Movement Disorders, 34(1), 48-57.
Marras, C., Canning, C. G., & Goldman, S. M. (2019). Environment, lifestyle, and Parkinson’s disease: implications for prevention in the next decade. Movement Disorders, 34(6), 801-811.
Palacios, N., Gao, X., McCullough, M. L., Schwarzschild, M. A., Shah, R., Gapstur, S., & Ascherio, A. (2012). Caffeine and risk of Parkinson’s disease in a large cohort of men and women. Movement Disorders, 27(10), 1276-1282.
Yang, F., Trolle Lagerros, Y., Bellocco, R., Adami, H. O., Fang, F., Pedersen, N. L., & Wirdefeldt, K. (2015). Physical activity and risk of Parkinson’s disease in the Swedish National March Cohort. Brain, 138(2), 269-275.
Zhang, D., Jiang, H., Xie, J., & Li, X. (2020). The association between dietary vitamin intake and the risk of Parkinson’s disease: a meta-analysis. Aging Clinical and Experimental Research, 32(9), 1661-1668.




